Does artificial intelligence have any role in healthcare in low resource settings?
Artificial intelligence (AI) has revolutionized healthcare in the past few decades (1). Initially being used solely as a medical decision support system, it is anticipated that AI has a potential role in personalized medicine, patient monitoring and improve health service delivery and management (2). AI has penetrated the health care domain rapidly in high income settings where an estimated USD 150 million could be saved with such applications in the next 5 years (3). However, there is limited literature available on its use in low resource settings.
Developing countries struggle with high burden of disease, lack of trained health care providers as well as poor healthcare delivery infrastructure (4,5). It is in such settings that AI has a tremendous role in reducing health inequity by early disease detection and diagnosis, improving the efficiency and the quality of existing healthcare services, reduce medical expenditure (6), and use task shifting to deliver services by community health workers (5).
We conducted an online survey of healthcare, engineering and business professionals regarding the use of AI in healthcare in low resource settings. This survey was conducted by a group of researchers at The Aga Khan University, Karachi, Pakistan who are actively involved in AI research (7). The purpose of this survey was to understand if local professionals thought AI has a potential role in the health industry, whether or not they had used this technology to solve a health issue and to understand the barriers of using AI in healthcare.
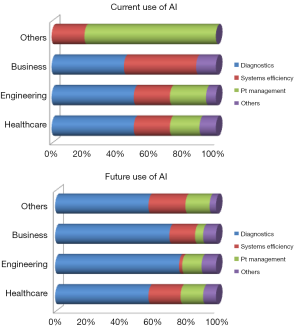
We received 368 responses during this survey. The average age of participants was 34 years (range, 16–72 years) with average work experience of 10 years (range, 3 months–45 years). Majority (n=233, 63%) of the respondents belonged to health care (physician, nurses as well as allied health staff) while the remaining included engineers (n=48, 13%), business professionals (n=55, 15%) and others (e.g., researchers, data analysts etc.) (n=35, 10%). Majority (n=250, 68%) of respondents had heard regarding the use of AI in healthcare. However, only 21% (n=78) had ever used AI to solve a healthcare problem. Professionals belonging to the field of health care were the most common users of AI (64%) followed by engineers (22%). The current and proposed uses of AI in healthcare according to the various professional disciplines have been shown in Figure 1.
AI use for diagnostic decision making was the most common response for current and future use of this technology among healthcare, engineering and business professionals. This was followed by the use of AI to improve systems efficiency (which included improvement in patient experience, management of workflow at the health facility etc.). Majority of the respondents (n=294, 80%) believed that AI could address health care affordability and accessibility issues.
Concerning the phenomenon of computers replacing human jobs, only 8.2% (n=30) of respondents felt that this was a concern. Majority of them (n=297, 81%) felt that AI would help augment human intelligence. When enquired about the hurdles to use AI, the most common reason cited by all professionals was lack of trained AI professionals (64%). The second most common hurdle cited by healthcare and engineering professionals was difficulty in identifying use cases (28%) while for the remaining respondents, cost of using this technology (22%) was a major concern. Approximately half the respondents (n=188, 51%) felt that they would be able to see an impact of AI in healthcare in Pakistan in the next 5 years.
Being reported from a low middle income country, this survey has re-emphasized the use of AI in healthcare irrespective of the socio-economic background of the region. Similar to Jiang et al., respondents in this survey also felt that diagnostic decision making was one of the key areas of impact for AI (2). This fact has been reported from low resource settings where computer based diagnostic systems for management of cardiovascular disease in India provided consistent recommendations (as compared to a physician) in more than 90% of the cases (5), thus improving healthcare access and ensuring quality for the marginalized populations. Despite the potential benefits of AI, the challenges for its widespread use remain consistent with the literature which include lack of training, infrastructure and cost issues (5).
With the Sustainable Development Goals only a decade away from completion (8), innovative technology in healthcare such as use of AI can improve access and quality of services to the most disadvantaged populations in low middle income countries, thus making the target of universal health care coverage achievable.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jmai.2019.06.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Horn W. AI in medicine on its way from knowledge-intensive to data-intensive systems. Artif Intell Med 2001;23:5-12. [Crossref] [PubMed]
- Jiang F, Jiang Y, Zhi H, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol 2017;2:230-43. [Crossref] [PubMed]
- Collier M, Fu R, Yin L, et al. Artificial intelligence: healthcare's new nervous system. Available online: https://accenture.com/t20170418T023006Z__w__/us-en/_acnmedia/PDF-49/Accenture-Health-Artificial-Intelligence.pdf. 2017
- Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health 2018;8:020303. [Crossref] [PubMed]
- Guo J, Li B. The Application of Medical Artificial Intelligence Technology in Rural Areas of Developing Countries. Health Equity 2018;2:174-81. [Crossref] [PubMed]
- Wahl B, Cossy-Gantner A, Germann S, Schwalbe NR. Artificial intelligence (AI) and global health: how can AI contribute to health in resource-poor settings?. BMJ Glob Health 2018;3:e000798. [Crossref] [PubMed]
- Hoodbhoy Z, Hasan B, Jehan F, Bijnens B, Chowdhury D. Machine learning from fetal flow waveforms to predict adverse perinatal outcomes: a study protocol. Gates Open Res 2018;2:8. [Crossref] [PubMed]
- UN. Sustainable development goal 3. [cited 2019 May 26]. Available online: https://sustainabledevelopment.un.org/sdg3
Cite this article as: Hoodbhoy Z, Hasan B, Siddiqui K. Does artificial intelligence have any role in healthcare in low resource settings? J Med Artif Intell 2019;2:13.